You Are What You Eat and Where You Eat It: Health Determinants and the Gut Microbiomes in Europe
“In food excellent medicine can be found” (Hippocrates 300 BC).
“Tell me what you eat, and I will tell you what you are” (Brillat-Savarin 1792).
“Man is what he eats” (Feuerbach 1825).
While these quotes are grounded in the philosophical teaching that food influences one’s state of mind, today, more than ever, we can appreciate the literal meaning of the words, “you are what you eat.” Indeed, while nutritional and medical advice continues to shape our understanding of how the gut microbiome promotes health or disease there is an increased appreciation for not only what people eat, but for where they eat it. Across Europe, where people live, learn, work, play, and worship are equally as influential to health. To that end, data centered consensus in social and economic policy making should always account for health and health equity within the mileu of the communities they look to serve. This is especially true when we examine the impact of health determinants and how they shape gut microbiomes across Europe.
The gut microbiome is as unique as fingerprints, weighs about 3kg (6 lbs.), and is composed of both good and bad bacteria. Together, these bacteria have been shown to influence health in positive and negative ways. For example, bad bacteria in the gut have been shown to influence diseases such as heart disease, cancer, neurodegenerative disorders, and diabetes. As we continue to learn more about the many factors that shape the microbiome, we are also beginning to understand how influential it is in shaping human health and well-being. These factors and forces are often referred to as “determinants of health.” These can be both social and biological. While some of these factors can be individually controlled—such as nutrition and exercise—there are many others that we have less control, such as when and where we are born, grow up, live, and work. Collectively, in Europe, these determinants are often collaboratively defined, researched, and widely influenced by scientific, health, and government services such as the European Center for Disease Control (ECDC), European Research Council (ERC), and the World Health Organization (WHO). Whether locally or across Europe these collaborative efforts look to improve health outcomes worldwide. While this ongoing work is massive in its scope (Figure 1), it is important to, first, zoom in on how the gut microbiome influences disease generally, and second, look at how, in Europe, specifically social and biological factors uniquely shape the health of the population there compared to global counterparts.
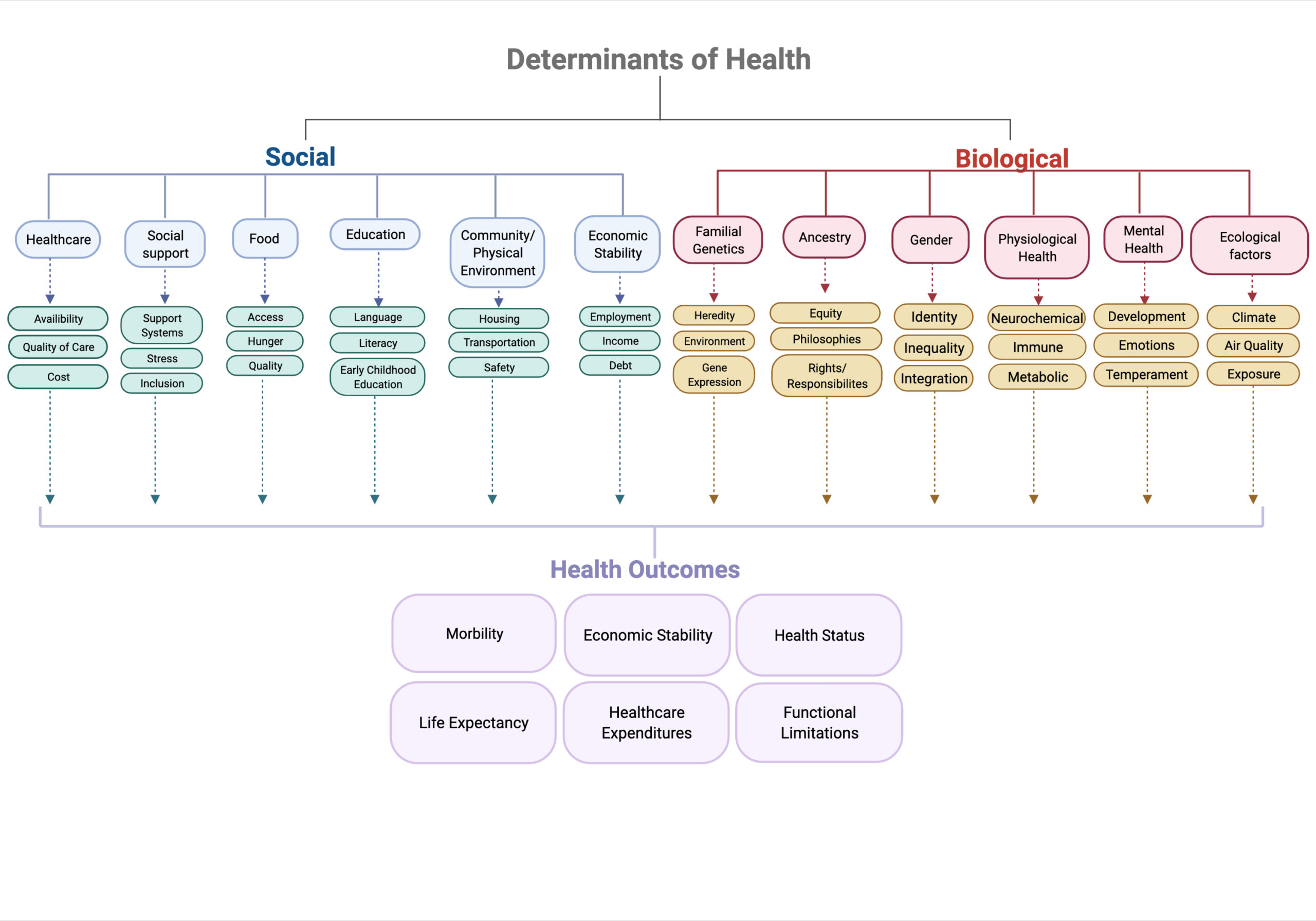
Figure 1 Determinants of health thought to influence the gut microbiome and human health globally
The state of gut microbiome research in Europe
What does the term microbiome mean? We define it as the community of bacteria, fungi, and viruses that share body space in humans. Further, the microbiome is often defined by where it is located, such as the skin, mouth, lung, cervix, or gut. The gut microbiome is particularly interesting because it is home to the largest number of bacteria in the whole body. Totaling roughly 100 trillion microbes, these bacteria represent as many as 5,000 different species and have approximately 300 times more DNA than the human genome. The role these diverse and abundant bacteria play in humans’ daily lives is only beginning to be understood, but scientists know that the gut plays a key role in metabolic, immunological, and neurologic processes. Exciting work is ongoing worldwide, with leading work being done in Europe to better understand how we might utilize the gut microbiome to improve health and to prevent maladaptive states such as cancer, neurodegeneration, and autoimmunity (Figure 2). Given the rapid advancement of microbiome research, we must also address the ethical and social implications that this research and its technology has had on public health and policy (for example, considering how broad manipulation of the gut microbiome would affect the collective microbiome of a community in a resource-poor versus a resource-rich area).
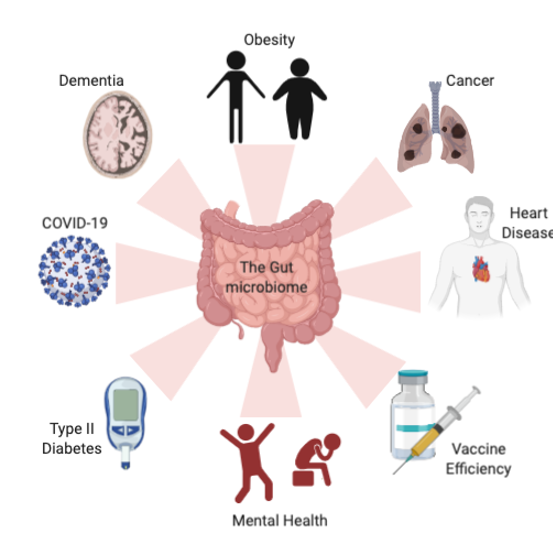
Figure 2 The microbiome influences multiple disease
The role of the microbiome in the fight against cancer
Cancer is the second leading cause of death in Europe with nearly 4 million new cases each year and approximately two million deaths. Recent work led by French, Italian, and German scientists at the Gustave Roussy Cancer Center, the Université de Paris-Sud, and the Institut national de la santé et de la recherche demonstrated that key bacteria present in tumors and in the gut may shape how patients respond to various treatment plans. Moreover, collaborative international work that studied patients with the same types of cancer (breast, lung, and skin) who received the same type of treatment had unique gut microbiome signatures that guided researchers to better understand where the patients lived. That is to say, the researchers saw that while the gut microbiome of breast cancer patients from the same country looked similar, it was very different from that of people in other countries. Specifically, the bacteria in the gut microbiome of cancer patients in Europe was very different from that of patients in the United States. This important scientific discovery showed for the first-time that where people live directly influenced how they might respond to cancer treatments such as chemotherapy. Furthermore, it highlighted the complexities involved when trying to study the gut microbiome. In light of this work, the EU recently provided 40 million euros to fund collaborative European efforts to study the gut microbiome and Europe is leading new advances in understanding the role of the gut microbiome in cancer that will allow scientist, physicians, and researchers to investigate innovative ways to target, track, and prevent cancer.
Influence of the microbiome on mental health and neurodegeneration
Much of what we have learned about the gut microbiome in oncology has furthered an understanding of the interface between the human nervous system and the gut microbiome, termed the gut-brain axis (GBA). This is an emerging field of microbiome research for which Europe has led funding since 2019 and the creation of project MINERVA (MIcrobiota-Gut-BraiN EngineeRed platform to eVAluate intestinal microflora impact on brain functionality). This European initiative has produced new insights and applications around understanding how the gut and the brain are linked, suggesting that the health of the gut microbiome influences mental and physical brain health. This is of immense importance to Europe where mental disorders are some of the most significant public health challenges affecting 50 percent of individuals across the entire region. Mental health disorders are also the leading cause of disability and the third leading cause of disease burden after cardiovascular disease and cancer.
To address the underlying causes of mental health, the University of Milan and others have shown that the gut and the brain communicate to direct the nervous system and our behavior. Moreover, fundamentally this is regulated by key bacteria that are present or absent in the gut microbiome. Importantly, the GBA exists in a delicate equilibrium, so that small changes to the gut microbiome can elicit behavioral changes—such as aggression or decreased stress—and vice versa. Recent studies in mice lacking a gut microbiome versus mice with a healthy gut microbiome revealed that the first group had a significantly higher presence of anxiety-like behaviors. Taken together, we begin to imagine how the positive identification of good bacteria populations in the gut microbiome could be used as an interventional therapeutic to improve, prevent, and treat mental health across Europe.
In discussing the impact the gut microbiome has on the brain it is also important to discuss maladaptive states of the brain such as Alzheimer’s and Parkinson’s. Europe has a rapidly aging population with 25 percent of the European population over the age of sixty-five. By 2030 it is expected that 12 percent of all deaths in Europe will be attributable to neurological disorders. While there is no current understanding about how the gut microbiome drives brain health or disease, it is suggested that diet, genetics, and other health metrics―such as where people live―contribute to high variability in these conclusions. For example, populations that lack access to fresh food, healthcare, and social services are more likely to suffer from chronic inflammatory disease states; this is in sharper focus when Europe is compared to the United States where there are high rates of food deserts, cost-prohibitive healthcare, and a lack of social services. Scientific and public health research continues to explore how societies can better address the dynamic equilibrium that exists between the gut microbiome, mental well-being, and brain health.
Impact of negative bacteria on obesity and diabetes
The prevalence of obesity is an increasing public health issue in developed and developing countries. It remains a pressing concern not just due to the implications it has on mortality but also because of the severe financial strain it puts on the healthcare system; estimated to cost 8 percent of Europe’s total health expenditures. In Europe, recent estimates show that 30-70 percent of the population is overweight, while 10-30 percent of the European population is obese. A recent study predicted that, by 2030, there will be around a 30 percent increase in obesity prevalence and a 130 percent increase in severe obesity prevalence worldwide, in addition to an increase in non-communicable comorbidities, such as cardiovascular disease, hypertension, and diabetes. Obesity is known to be influenced by a number of factors, such as diet, physical activity, genetics, and environment. Recent studies have demonstrated that overweight or obese patients are more likely to have negative bacteria in their gut that may contribute to decreased energy and metabolism and lead to insulin resistance. This may account for why we continue to see increases in heart disease and diabetes in Europe. While this biology clearly warrants further investigation, Europeans can boost healthy bacteria in their gut to improve personal health by increasing fiber intake, decreasing processed food and meat intake, and increasing fresh fruit and vegetables intake. While somewhat controversial, it is recommended to forgo over-the-counter probiotics and substitute those for fiber, leafy greens, and naturally occurring healthy bacteria in fermented food, such as yogurt, sauerkraut, tempeh, kimchi, miso, and pickles. These are among the foods that are thought to directly affect host immunity and gut health. Many of these foods are regularly consumed as part of regional diets across Europe and have been shown to positively impact the health of the microbiome.
Physical and social determinants of disease
Because cancer, neurodegeneration, and obesity remain leading causes of death in Europe, it is important to understand not only their biological causes, but also the social factors that may play a major role in European and global health (Figure 2), such as social support programs, education, and the environment. While people are not in control of where they are born and grow up, sometimes they can be actively involved in what they eat, or how much they exercise and sleep. Additionally, the local, state, federal, and multinational governments have a large role to play in shaping and investing in social and biological programs that improve human health. When comparing Europe with the rest of the world, how do diet, physical environment, education, social support, and wealth inequality influence health and in particular the microbiome?
The role of the environment in promoting microbiome health
Among major social and physical determinants of health, the physical environment is one of the most important indicators of long-term health. Physical environment encompasses urban setting, pollution, water quality, noise, and more. Collectively, these factors play a vital role in shaping the health of the gut microbiome and in turn people’s health and well-being. Chronic exposure to unsafe drinking water, airborne pollutants, and other environmental toxins are known pollutants of the gut microbiome. Moreover, one in every eight deaths in Europe is attributed to environmental factors. These deaths are preventable and could be significantly reduced if the EU and individual countries implemented key sustainable environmental policy protections that are known to impact the health of our microbiome.
In addition to air quality contributing to human health, water quality is also a key metric of gut health. Water quality has been an increasing concern as global agriculture requires the use of more nutrients resulting in increased nitrate levels in common water supply. Increased nitrate levels have been associated with various cancer subtypes such as colorectal cancer because of how readily absorbed nitrate in the gut microbiome causes inflammation in the gut and a suppression of the immune system. Although, European countries have exceptional water quality (as defined by quality standards related to physical and chemical properties) and lower air pollution (as defined by emissions, chemicals, dust, ozone, etc.) when compared to other G20 countries there remain shortcomings that are difficult to surmount as the co-coordination of European policy protection of air and water vary from country to country.
The role of social support and social mobility in public health
Research has consistently demonstrated welfare programs and social mobility have a positive impact on the gut microbiome and in our health, and well-being. Moreover, stress, diet, and trauma are more frequently experienced by those who lack social support and mobility, which in turn lead to negative mental and physical health. Many European nations, such as Denmark, Norway, and Finland, lead these efforts globally, while other such as Latvia, Estonia, and Germany have quite a bit of room to improve. Moreover, Europe consistently beats out the United States, China, India, and Japan in its longstanding commitment to social support programs. To that end, mitigating widespread poverty with robust social safety nets are likely to improve the gut microbiomes and public health outcomes of countries across Europe.
Where people are born, grow up, work, and live clearly plays a large role in shaping their well-being. For example, Europeans are more likely to have better access to healthcare, education, and social support programs when compared to the average citizens of United States, China, or India. This has been shown to increase life expectancy, quality of life, and happiness. However, should people have the means to take control of their health, there are a number of proactive ways they could care for their gut microbiome and personal health Although it is not always accessible to all and may remain a luxury for many, taking charge of one’s diet, focusing on high fiber, low sugar, and natural probiotic food help, as well as protecting one’s sleep, coping with stress and including exercise in a daily routine. Another useful avenue is to get involved in supporting local, state, and federal policies that enhance access to clean air, sustainable agriculture, social support programs, economic mobility, and education. As more is known about how the gut microbiome shapes human health, it will become increasingly evident how external biological and social factors play a key role. Until then, perhaps we will discover that we need the best that Europe has to offer- social support programs from Norway, healthcare from Denmark, air quality from Sweden and Finland, water from Switzerland, and healthy food from Spain. In the meantime, it may be time to reevaluate the famous mantra, “you are what you eat,” to be more inclusive of the social and biological determinates of health: “You are what you eat and where you eat it,” because what you eat is likely as important as where you eat it.
Alexandria Cogdill, MEng, PhD, is immunologist at the University of Texas MD Anderson Cancer Center and a Fulbright grantee working in Paris, France in affiliation with the Gustave Roussy Institut and the Institut National de la Santé et de la Recherche Médicale U1015. Dr. Cogdill’s work has furthered our understanding of how the immune system can be used to improve health and overcome disease. She has conducted cancer and immunology research at the National Institutes of Health, Harvard Medical School, and the University of Pennsylvania.
Zach Kulstad is a senior at Carleton College and a student researcher in the Cancer Prevention & Research Institute of Texas (CPRIT)-CURE summer program.
Jennifer Wargo, MD, MMSc is a Professor of Surgical Oncology and Genomic Medicine at the University of Texas MD Anderson Cancer Center in the departments of Surgical Oncology and Genomic Medicine. Dr. Wargo’s work has helped to define determinants of response and resistance to cancer therapy, including recent work defining the role of the gut and tumor microbiomes in cancer.
References:
Bercik, P., S. M. Collins, and E. F. Verdu. “Microbes and the Gut-Brain Axis.” Neurogastroenterol Motil 24, no. 5 (May 2012): 405-13.
Bowyer, R. C. E., M. A. Jackson, C. I. Le Roy, M. Ni Lochlainn, T. D. Spector, J. B. Dowd, and C. J. Steves. “Socioeconomic Status and the Gut Microbiome: A Twinsuk Cohort Study.” Microorganisms 7, no. 1 (Jan 11 2019).
Diaz Heijtz, R., S. Wang, F. Anuar, Y. Qian, B. Bjorkholm, A. Samuelsson, M. L. Hibberd, H. Forssberg, and S. Pettersson. “Normal Gut Microbiota Modulates Brain Development and Behavior.” Proc Natl Acad Sci U S A 108, no. 7 (Feb 15 2011): 3047-52..
Dobbs, S. M., R. J. Dobbs, C. Weller, A. Charlett, A. Augustin, D. Taylor, M. A. Ibrahim, and I. Bjarnason. “Peripheral Aetiopathogenic Drivers and Mediators of Parkinson’s Disease and Co-Morbidities: Role of Gastrointestinal Microbiota.” J Neurovirol 22, no. 1 (Feb 2016): 22-32..
Dowd, J. B., and A. Renson. ““Under the Skin” and into the Gut: Social Epidemiology of the Microbiome.” Curr Epidemiol Rep 5, no. 4 (2018): 432-41.
Evans, G. W., and P. Kim. “Childhood Poverty and Health: Cumulative Risk Exposure and Stress Dysregulation.” Psychol Sci 18, no. 11 (Nov 2007): 953-7.
Finkelstein, E. A., O. A. Khavjou, H. Thompson, J. G. Trogdon, L. Pan, B. Sherry, and W. Dietz. “Obesity and Severe Obesity Forecasts through 2030.” Am J Prev Med 42, no. 6 (Jun 2012): 563-70.
Gopalakrishnan, V., B. A. Helmink, C. N. Spencer, A. Reuben, and J. A. Wargo. “The Influence of the Gut Microbiome on Cancer, Immunity, and Cancer Immunotherapy.” Cancer Cell 33, no. 4 (Apr 9 2018): 570-80.
Gopalakrishnan, V., C. N. Spencer, L. Nezi, A. Reuben, M. C. Andrews, T. V. Karpinets, P. A. Prieto, et al. “Gut Microbiome Modulates Response to Anti-Pd-1 Immunotherapy in Melanoma Patients.” Science 359, no. 6371 (Jan 5 2018): 97-103.
Hahn, R. A., and B. I. Truman. “Education Improves Public Health and Promotes Health Equity.” Int J Health Serv 45, no. 4 (2015): 657-78.
Houser, M. C., and M. G. Tansey. “The Gut-Brain Axis: Is Intestinal Inflammation a Silent Driver of Parkinson’s Disease Pathogenesis?”. NPJ Parkinsons Dis 3 (2017): 3.
Kampa, M., and E. Castanas. “Human Health Effects of Air Pollution.” Environ Pollut 151, no. 2 (Jan 2008): 362-7.
Kawachi, I., and B. P. Kennedy. “Income Inequality and Health: Pathways and Mechanisms.” Health Serv Res 34, no. 1 Pt 2 (Apr 1999): 215-27.
Leach, S. A., M. Thompson, and M. Hill. “Bacterially Catalysed N-Nitrosation Reactions and Their Relative Importance in the Human Stomach.” Carcinogenesis 8, no. 12 (Dec 1987): 1907-12.
Low, M. D., B. J. Low, E. R. Baumler, and P. T. Huynh. “Can Education Policy Be Health Policy? Implications of Research on the Social Determinants of Health.” J Health Polit Policy Law 30, no. 6 (Dec 2005): 1131-62.
Mason, K. L., G. B. Huffnagle, M. C. Noverr, and J. Y. Kao. “Overview of Gut Immunology.” Adv Exp Med Biol 635 (2008): 1-14.
Matson, V., J. Fessler, R. Bao, T. Chongsuwat, Y. Zha, M. L. Alegre, J. J. Luke, and T. F. Gajewski. “The Commensal Microbiome Is Associated with Anti-Pd-1 Efficacy in Metastatic Melanoma Patients.” Science 359, no. 6371 (Jan 5 2018): 104-08.
Neufeld, K. M., N. Kang, J. Bienenstock, and J. A. Foster. “Reduced Anxiety-Like Behavior and Central Neurochemical Change in Germ-Free Mice.” Neurogastroenterol Motil 23, no. 3 (Mar 2011): 255-64, e119.
Pluta, R., M. Ulamek-Koziol, S. Januszewski, and S. J. Czuczwar. “Gut Microbiota and Pro/Prebiotics in Alzheimer’s Disease.” Aging (Albany NY) 12, no. 6 (Mar 19 2020): 5539-50. https://doi.org/10.18632/aging.102930.
Poore, G. D., E. Kopylova, Q. Zhu, C. Carpenter, S. Fraraccio, S. Wandro, T. Kosciolek, et al. “Microbiome Analyses of Blood and Tissues Suggest Cancer Diagnostic Approach.” Nature 579, no. 7800 (Mar 2020): 567-74.
Reblin, M., and B. N. Uchino. “Social and Emotional Support and Its Implication for Health.” Curr Opin Psychiatry 21, no. 2 (Mar 2008): 201-5.
Routy, B., E. Le Chatelier, L. Derosa, C. P. M. Duong, M. T. Alou, R. Daillere, A. Fluckiger, et al. “Gut Microbiome Influences Efficacy of Pd-1-Based Immunotherapy against Epithelial Tumors.” Science 359, no. 6371 (Jan 5 2018): 91-97.
Sharma, S., and P. Tripathi. “Gut Microbiome and Type 2 Diabetes: Where We Are and Where to Go?”. J Nutr Biochem 63 (Jan 2019): 101-08.
Totelin, L. “When Foods Become Remedies in Ancient Greece: The Curious Case of Garlic and Other Substances.” J Ethnopharmacol 167 (Jun 5 2015): 30-7.
Turnbaugh, P. J., R. E. Ley, M. A. Mahowald, V. Magrini, E. R. Mardis, and J. I. Gordon. “An Obesity-Associated Gut Microbiome with Increased Capacity for Energy Harvest.” Nature 444, no. 7122 (Dec 21 2006): 1027-31.
Whelton, A. J., L. McMillan, M. Connell, K. M. Kelley, J. P. Gill, K. D. White, R. Gupta, R. Dey, and C. Novy. “Residential Tap Water Contamination Following the Freedom Industries Chemical Spill: Perceptions, Water Quality, and Health Impacts.” Environ Sci Technol 49, no. 2 (Jan 20 2015): 813-23.
Photo: Microbiome inside a human body in a protecting shining shell | Shutterstock
Published on April 1, 2021.




